Articles
Hypercalcaemia in an elderly dog
10th December 2021
A 30kg, 11 year old male neutered crossbreed presented with two month history of progressive polydipsia and polyuria. No abnormal findings were noted on the physical examination.
Hypercalcaemia (Total calcium 3.4 mmol/l) was noted on biochemistry. Urinalysis revealed a low urine S.G. (1.010), with no other abnormalities.
The list of differentials for hypercalcaemia is long although many can be eliminated easily when assessed in conjunction with the rest of the blood test results, the history and physical examination (Table 1). The most common pathological cause of hypercalcaemia in the dog is humeral hypercalcaemia of malignancy with lymphoma being the most common malignant cause of hypercalcaemia. In most cases diagnostic imaging is the next port of call in pursuit of a diagnosis – a so-called ‘tumour hunt’.
| Table 1 |
| Causes of hypercalcaemia |
| Non-pathological |
| · Non-fasting (minimal elevation), physiologic (growth in young animals), hyperlipidaemia, laboratory error)
· Transient causes: Hyperproteinaemia, haemoconcentration, severe hypothermia (rare) |
| Pathological |
| · Parathyroid dependant – hyperparathyroidism
· Parathyroid independent – malignancy, idiopathic, hypervitaminosis D, renal failure, granulomatous disease, hyperadrenocorticism, skeletal abnormalities, grape toxicity, calcium supplementation, DMSO, phosphate binders with high calcium content. |
Lateral thoracic radiographs (Figure 1) revealed a large soft tissue opacity in the cranial thorax and the DV projection confirmed this to lie within the mediastinum. Abdominal projections were unremarkable. Differentials for a mediastinal mass are listed in Table 2.
| Table 2 |
| Differentials for a cranial mediastinal mass |
| · Thymoma
· Lymphoma · Ectopic thyroid or parathyroid tissue · Chemodectoma · Metastatic neoplasia · Granuloma · Thymic branchial cyst · Branchial cyst carcinoma |
Ultrasound-guided FNA samples yielded predominantly small lymphocytes with occasional intermediate and large lymphocytes. No epithelial cells were noted although the predominance of small lymphocytes was suggestive of thymoma. Flow cytometry confirmed a diagnosis of thymoma (>10% CD4+CD8+ lymphocytes). (Cytology 1 and 2) CT imaging (Figure 2) was undertaken prior to surgery revealed the mass to be large but well defined with no evidence of invasion or pulmonary metastasis and no lymphadenomegaly.
The mass was removed by means of a midline thoracotomy and histology confirmed the tumour to be a thymoma. Recovery was uneventful and hypercalcaemia along with PUPD had resolved within a week of surgery. At last contact 18 months later the patient remained clinically well.

Figure 1
Ventrodorsal thoracic
radiograph with a
mediastinal mass
cranial to the heart.

Figure 2
Transverse postcontrast
CT image of
the mediastinal mass.
Differentiation between thymoma and thymic lymphoma can sometimes be achieved by means of FNA samples but in both cases lymphocytes are the predominant cell type. Thymoma frequently resembles a normal lymph node, containing a mixed population of lymphoctyes, but predominantly small lymphocytes. Mast cells are also common in small numbers. Cytology 1. Shows an example of cytology from a thymoma.
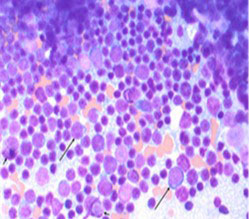
Cytology 1
FNA from a thymoma in a dog (not the
patient in this case). Nucleated cells
consist predominantly of small
lymphocytes. Low numbers of intermediate
to large lymphocytes (long arrows)
and occasional individual mast cells
(short arrows) are also observed.*
The malignant clone within the thymoma is of epithelial cells and if these are not evident on cytology, repeat sampling, PARR, flow cytometry or histology may be required to make the diagnosis.
By contrast, thymic lymphoma is made up of a malignant clone of lymphocytes, most commonly large lymphocytes and the image would more closely resemble that seen in Cytology 2.
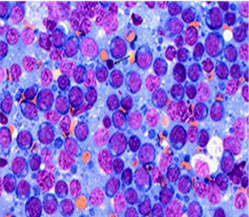
Cytology 2
By contrast, thymic lymphoma presents
with predominantly intermediate to
large lymphocytes as seen in this FNA
(from a lymph node of a patient with
lymphoblastic lymphoma).*
* Images from Viesselmann, L, 2019, https://www.dvm360.com/view/thymoma-11-year-old-dogclinicalpathology-perspective
Back to news & events



